Our Advanced Endoscopy Centre is equipped with the latest technology for minimally invasive diagnostic and therapeutic procedures. We specialize in the early detection and treatment of gastrointestinal (GI) disorders, ensuring precision, safety, and patient comfort.
- Colonoscopy – Detailed evaluation of the colon and rectum for polyps, cancer screening, and inflammatory bowel disease (IBD).
- Endoscopic Polypectomy – Safe removal of polyps to prevent colorectal cancer.
- Endoscopic Biopsy – Tissue sampling for accurate diagnosis of gastrointestinal diseases.
- Endoscopic Hemostasis – Stopping GI bleeding with advanced techniques.
- ERCP (Endoscopic Retrograde Cholangiopancreatography) – Diagnosis and treatment of bile duct and pancreatic disorders.
- Capsule Endoscopy – Non-invasive, pill-sized camera technology for small intestine imaging.
Early detection, precise treatment, and expert care for better digestive health.
Colonoscopy – Detailed evaluation of the colon and rectum for polyps
cancer screening, and inflammatory bowel disease (IBD)
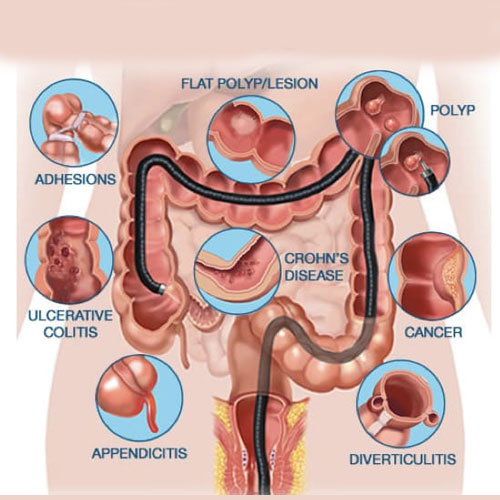
Introduction to Colonoscopy
Colonoscopy is a diagnostic procedure that allows doctors to closely examine the inner lining of the colon and rectum using a flexible, tube-like instrument called a colonoscope. It plays a vital role in identifying abnormalities such as polyps, tumors, inflammation, and bleeding. This procedure is often recommended for cancer screening, especially for individuals over the age of 45 or those with a family history of colorectal cancer. Colonoscopy helps detect problems at an early stage, increasing the chances of successful treatment and prevention.
Screening for Polyps and Cancer
One of the primary purposes of a colonoscopy is the early detection and removal of polyps, which are small growths that can potentially develop into cancer over time. During the procedure, if any polyps are found, they can often be removed immediately and sent for biopsy. Early removal greatly reduces the risk of colorectal cancer. For patients with symptoms such as rectal bleeding, unexplained weight loss, or persistent abdominal pain, colonoscopy provides a thorough and accurate evaluation.

Diagnosis of Inflammatory Bowel Disease (IBD)
Colonoscopy is essential for diagnosing and managing inflammatory bowel diseases like Crohn’s disease and ulcerative colitis. These chronic conditions cause inflammation in the digestive tract and require regular monitoring to assess disease activity and response to treatment. The procedure allows doctors to take tissue samples (biopsies) to confirm the diagnosis and guide medication choices. Colonoscopy also helps in detecting complications of IBD, such as strictures, ulcers, or dysplasia.
Preparation and Recovery
Before a colonoscopy, patients must follow a bowel preparation process to clear the colon, usually involving a special diet and laxatives. The procedure is typically performed under sedation to ensure comfort. Most colonoscopies are completed within 30–60 minutes, and patients can usually return home the same day. Minor side effects like bloating or cramping may occur but resolve quickly. Colonoscopy is considered safe and is a key tool in maintaining gastrointestinal health and preventing serious disease.
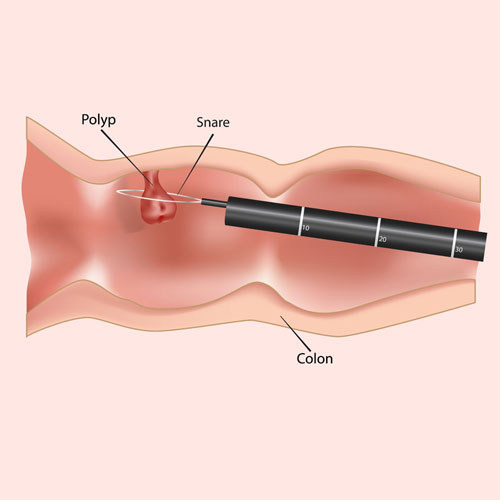
Endoscopic Polypectomy
Safe removal of polyps to prevent colorectal cancer
Introduction to Endoscopic Polypectomy
Endoscopic polypectomy is a medical procedure used to remove polyps from the lining of the colon or rectum during a colonoscopy. Polyps are abnormal tissue growths that can be benign, pre-cancerous, or cancerous. Removing them early plays a crucial role in preventing colorectal cancer. The procedure is minimally invasive, performed using a flexible endoscope equipped with specialized tools that allow doctors to visualize and safely excise polyps without open surgery.
Why It’s Important
Most colorectal cancers begin as polyps, which may grow silently without causing symptoms. Endoscopic polypectomy helps identify and remove these growths before they become dangerous. It is often performed as part of routine colon cancer screening, especially in individuals over 45 or those with a family history of colorectal disease. By catching and eliminating polyps early, the risk of developing colorectal cancer is significantly reduced.
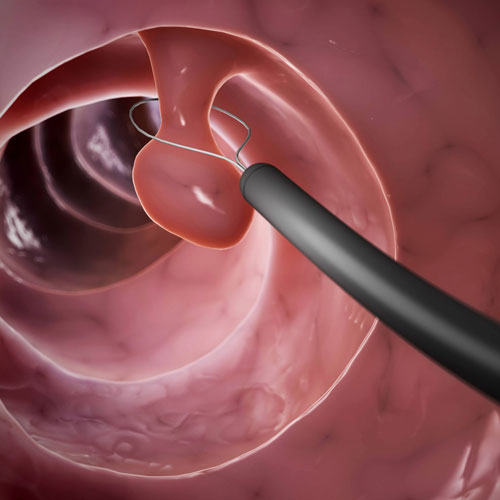
How the Procedure Works
During a colonoscopy, if a polyp is detected, the doctor uses tools passed through the endoscope to snare or cut the polyp from the colon wall. Smaller polyps are often removed with a wire loop or biopsy forceps, while larger ones may require electrocautery or injection-assisted techniques. The removed tissue is then sent to a lab for histopathological analysis to determine its nature and guide further treatment if necessary.
Safety and Recovery
Endoscopic polypectomy is considered safe and effective, with a low risk of complications. Most patients experience little to no discomfort and can resume normal activities within a day. Rarely, there may be mild bleeding or, in rare cases, a small perforation that requires additional treatment. Post-procedure instructions usually include avoiding certain foods and activities for a short period. Regular follow-up colonoscopies may be recommended to monitor for new polyps and maintain colon health.
Endoscopic Biopsy
Tissue sampling for accurate diagnosis of gastrointestinal diseases
Introduction to Endoscopic Biopsy
An endoscopic biopsy is a procedure where small tissue samples are taken from the lining of the gastrointestinal (GI) tract during an endoscopy. This minimally invasive technique is essential for diagnosing various GI conditions, including inflammation, infections, ulcers, and cancers. The biopsy is performed using specialized instruments passed through the endoscope, allowing doctors to target suspicious areas precisely. It provides critical information that cannot be obtained through visual inspection alone.
Why It’s Performed
Doctors recommend an endoscopic biopsy when abnormalities are detected in the esophagus, stomach, small intestine, or colon. Conditions like celiac disease, Helicobacter pylori infection, Crohn’s disease, and GI cancers often require microscopic examination of tissue for confirmation. The biopsy helps differentiate between benign and malignant changes and guides the choice of treatment. It is a key tool in early detection and accurate diagnosis of serious gastrointestinal diseases.
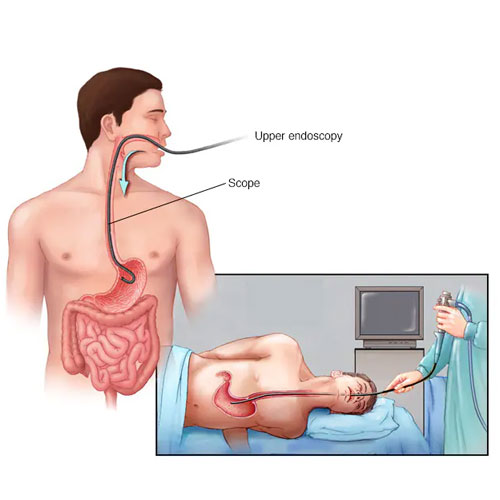
Procedure Details
During an upper or lower GI endoscopy, the doctor gently inserts an endoscope through the mouth or rectum to visualize the digestive tract. When an abnormality is seen, a small forceps or snare is used to extract tissue samples from the affected site. The samples are preserved and sent to a pathology lab, where they are analyzed under a microscope. The procedure is generally painless and done under sedation, with the entire process taking less than an hour.
Recovery and Follow-Up
Recovery from an endoscopic biopsy is usually quick, with most patients resuming normal activities within a few hours. Some may experience mild throat soreness or bloating, depending on the type of endoscopy performed. Results from the biopsy are typically available within a few days and help determine the next steps in treatment. Whether confirming a diagnosis or ruling out a serious condition, endoscopic biopsy is a safe and effective method to ensure precise and timely medical care.

ERCP (Endoscopic Retrograde Cholangiopancreatography)
Diagnosis and treatment of bile duct and pancreatic disorders
Introduction to ERCP
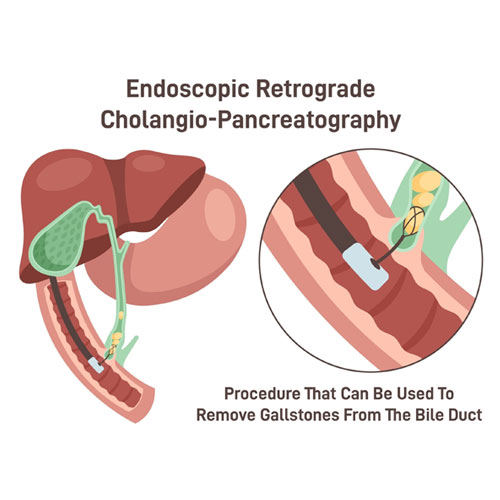
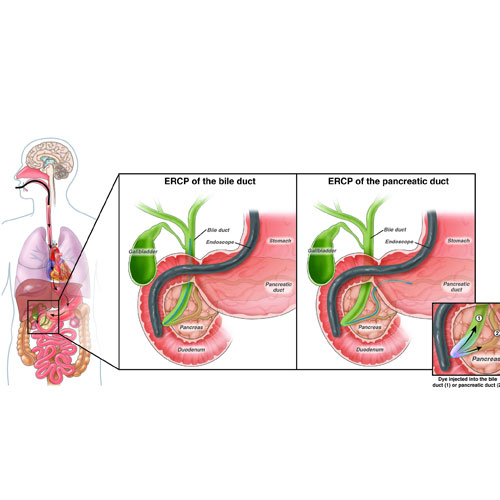
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a specialized procedure used to diagnose and treat conditions affecting the bile ducts, gallbladder, and pancreas. It combines endoscopy with fluoroscopy (X-ray imaging) to provide detailed views of these structures. ERCP is typically recommended when symptoms such as jaundice, abdominal pain, or abnormal liver function tests suggest a blockage or disorder in the biliary or pancreatic ducts. It not only helps in diagnosing the issue but also allows for immediate therapeutic intervention.
How ERCP Works
During ERCP, a flexible endoscope is passed through the mouth, esophagus, and stomach into the first part of the small intestine (duodenum). A special catheter is then inserted through the scope to inject contrast dye into the bile and pancreatic ducts, making them visible on X-ray. If any abnormalities like stones, strictures, or tumors are detected, tools can be passed through the endoscope to treat them during the same session. This makes ERCP both a diagnostic and therapeutic procedure.
Common Uses and Treatments
ERCP is widely used to remove gallstones from the bile ducts, place stents to relieve ductal obstructions, and take biopsies for cancer diagnosis. It is also used to dilate narrowed ducts and treat leaks or infections associated with pancreatitis or bile duct injuries. These interventions can provide immediate symptom relief and prevent more serious complications. ERCP is especially valuable in cases where other imaging tests like MRI or CT scans are inconclusive.
Safety and Recovery
ERCP is generally safe when performed by experienced specialists, but it does carry some risks, such as pancreatitis, infection, or bleeding. Patients are usually monitored for a few hours after the procedure and may go home the same day if no complications arise. Mild throat discomfort or bloating may occur temporarily. Recovery is typically quick, and results from any biopsies are shared within a few days. ERCP plays a vital role in managing complex biliary and pancreatic conditions with both precision and efficiency.
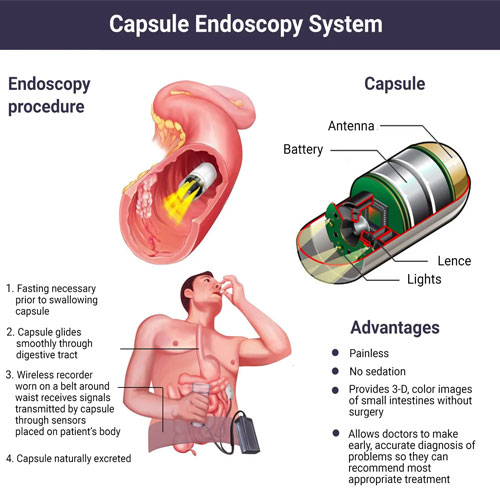
Capsule Endoscopy
Non-invasive, pill-sized camera technology for small intestine imaging
Introduction to Capsule Endoscopy
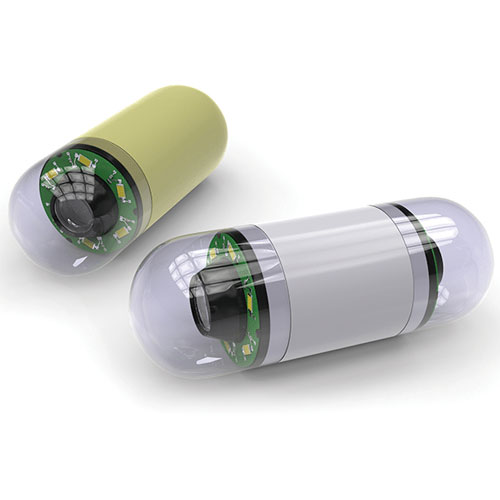
Capsule endoscopy is a non-invasive diagnostic procedure that uses a small, pill-sized camera to capture images of the gastrointestinal (GI) tract, particularly the small intestine. This innovative technology is designed to detect abnormalities that are difficult to reach with traditional endoscopy or colonoscopy. It is especially useful for evaluating unexplained bleeding, suspected Crohn’s disease, or small bowel tumors. The procedure is safe, painless, and does not require sedation or hospitalization.
How the Procedure Works
The patient swallows a vitamin-sized capsule that contains a tiny camera, light source, and transmitter. As the capsule travels naturally through the digestive tract, it takes thousands of images, which are transmitted to a recorder worn on a belt. These images are later reviewed by a specialist to identify any issues such as inflammation, ulcers, bleeding, or tumors. The capsule is disposable and exits the body naturally during a bowel movement within a day or two.
Common Uses and Benefits
Capsule endoscopy is most commonly used when other imaging tests have not provided a clear diagnosis. It is especially effective for identifying sources of gastrointestinal bleeding or diagnosing conditions like celiac disease and small bowel cancer. Because the capsule travels through the entire small intestine, it provides a comprehensive view that traditional endoscopy cannot reach. The procedure is patient-friendly, with no need for invasive instruments or recovery time.
Safety and Considerations
Capsule endoscopy is considered very safe, with minimal risk of complications. However, it may not be suitable for patients with bowel obstructions or swallowing difficulties. In rare cases, the capsule may get stuck in a narrowed area of the intestine, which might require surgical removal. Patients are usually advised to avoid eating or drinking for a few hours before and after swallowing the capsule. Overall, capsule endoscopy is a highly effective tool for diagnosing complex small intestine disorders in a comfortable, non-invasive way.